You Always get the best Guidance
Dr. R. Ramnarayan
Consultant Restorative / Functional Neurosurgeon
- M.B.B.S: Medical College, Trivandrum, University of Kerala, India.
- M.Ch (Neurosurg), National Institute of Mental Health and NeuroSciences (NIMHANS). Bangalore, India.
- Clinical attachment from Singapore General hospital.
- Functional Neurosurgery Fellowship from the Walton Centre for Neurology and Neurosurgery, Liverpool, United Kingdom.
- F.R.C.S - conferred by the Royal College of Surgeons of England, London.
- IFAANS conferred by the American Association of Neurological Surgeons.
About Restorative Neurosurgery
Neurosurgery is that branch of medicine dealing with surgical treatment of diseases in the brain and spinal cord. This includes surgery for patients with tumours of the brain and spinal cord, surgery for disorders of the blood vessels of the brain like aneurysms, surgery for all types of strokes including putaminal haematoma, surgery for spinal problems like disc prolapse, neurological problems in children like brain tumours, congenital defects like meningocoel and hydrocephalus etc. Nowadays neurosurgery has advanced so much and has developed subspecialties like pediatric neurosurgery, spinal surgery, functional neurosurgery etc.
Functional neurosurgery is concerned with the treatment of conditions where central nervous system (brain and spinal cord) physiology (normal function) is altered but the anatomy may or may not be normal. Examples of conditions treated by functional neurosurgery are chronic pain (including cancer pain and failed back surgery syndrome), spasticity, movement disorders (Parkinson's disease, dystonia, tremor etc), psychiatric conditions and epilepsy etc. Recently addiction is being added as an indication.
Dr. R. Ramnarayan is a neurosurgeon now focusing entirely on Restorative / Functional neurosurgery for the last many years. Neurosurgery is that branch of medicines which deals with the surgical management of diseases of the brain, spinal cord and the nerves. It is now subdivided into many including vascular neurosurgery, paediatric neurosurgery, spine neurosurgery, restorative neurosurgery etc. Restorative neurosurgery is that subspecialisation of neurosurgery that deals with the surgical management of lost functions of the brain, spinal cord and the nerves. This includes surgery for various conditions like movement disorders (Parkinson's disease), for conditions like OCD, depression , autism, addictions including alcoholism, for patients with paralysis of one side of the body (hemiplegia) or both legs (paraplegia), for chronic pains including cancer pains and diabetic neuropathy, for lost control of urine and bowels etc.
Functional Neurosurgery
Functional neurosurgery is concerned with the treatment of conditions where central nervous system (brain and spinal cord) physiology (normal function) is altered but the anatomy may or may not be normal. Examples of conditions treated by functional neurosurgery are chronic pain (including cancer pain and failed back surgery syndrome), spasticity, movement disorders (Parkinson's disease, dystonia, tremor etc), psychiatric conditions and epilepsy etc. Recently addiction is being added as an indication. Read More...
Patients Talking About
Dr. R. Ramnarayan
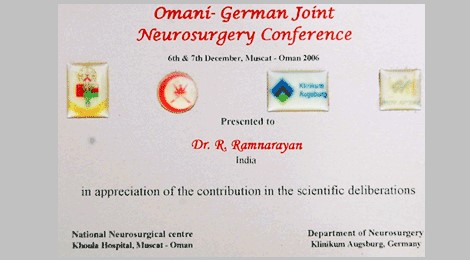
Awards Of
Dr. R. Ramnarayan
Patient Speaks
Testimonials
"My brother, age 60-years, was suffering from epilepsy since childhood and was on multiple medications. Over the years, he developed severe depression affecting his day-to-day life. We consulted several specialized doctors in the city who would continue adding more medications with very little clinical improvement. Being a surgeon myself, I was getting extremely frustrated with the deteriorating condition of my brother. In early 2020, a chance meeting with Dr. Ramnarayan, a renowned Consultant Restorative / Functional Neurosurgeon, practicing in Chennai proved to be a game-changer. In the very first meeting, I was impressed with the tremendous work he is doing in this ‘rare and highly specialized field’ with extremely favourable outcomes. I did not think twice before subjecting my brother to ‘Vagal Nerve Stimulation’ surgery advised by him. Within few weeks of surgery, there was significant improvement in his clinical condition; the medications have been reduced, the frequency of seizures had come down, and so has the depression been controlled to a large extent. I can’t thank Dr. Ramnarayan enough for this outcome, and what stands out are his humble nature, ready smile and dexterous hands. At the end of the day, it is his work which speaks! Wishing him the very best to continue the good work and make significant difference o many lives who are silently suffering from mental health issues. Thanks a Ton, Dr. Ramnarayan! "
Dr. Manda Venkatramana, MS, FRCSEd, FRCS(Glasg)
"My Father Satyanarayana was suffering from Parkinson's since he was 64. After 3 years when medicines are not responding that well he was advised to go for a DBS surgery."
Srinivasa Rao
"My mother had been suffering from leg and back pain for many years. She tried various alternate therapies and treatments (such as Neuro-therapy, Chiropractic, etc.) to no effect. During one of such kind of this alternate therapy treatment she acquired a condition where she couldn't move her right foot and couldn't feel the fingers in her right leg."
Vidyashankar Natarajan
"I extend my sincerely gratitude to God Almighty and to Dr. R.Ramnarayan, consultant Functional neurosurgeon and his team in Apollo Specialty Hospital, Chennai, India. My son was suffering from Cervical Dystonia (Spasmodic Torticollis) for a few years now. He has also been slowly loosing his voice and was unable to talk."
Mr. Muhammed Younis
"My name is Mohammad Faiq Arif and belong to city of Peshawar which is the north capital city of the province Pakhtunkhwa pakisthan. My dad, mom and i have come to chennai for my dad check up after one year of deep Brain, simulation precedure and he is doing very well"
Faiq Arif
"Thanks, doctor, for the wonderful treatment you have given to my Dad. The operation and procedure were wonderful and successful. Thanks once again for the confidence and the motivation you gave us during and after the operation. Excellent job and I hope you will continue to serve other patients."
Mrs. Zeinab Haji
"I underwent DBS operation for parkinsonism in Apollo Specialty Hospital, Chennai on 20-02-2012 by Dr.R.Ramnarayan, Consultant neurosurgeon. I feel totally relieved from the previous parkinsonism effects. The tremor and the stiffness have gone very much and does of the drug has been reduced..."
Mr. Gnansigamoni
" I am Areef Hussain currently working in Singapore. My family stays in Nellore - Andhra Pradesh. My father Akbar Basha was diagnosed with Parkinson's disease from last 6 years. Recently his struggles got worsen as the effect of Syndopa tablets was reducing gradually. He had lot of troubles with severe body pains, walking difficulties and he was unable to perform day to day activities... "